Career Diaries: What It's Like to be a Counsellor in a Hospice

Name: Irene Lee
Occupation: Spiritual Care Counsellor at HCA Hospice Care
Age: 65
Years of experience: 38 years
Education background: Masters in Biblical Studies (Melbourne), Masters in Counselling (Singapore)
Years with current company: 4.5 years
Top 3 skills: Possess unconditional positive regard, have compassionate presence and ability to conduct Family Dignity Intervention.
Best lesson learned on the job: Presence and just being there for someone speaks louder than any action.
Why did you become a Counsellor?
Many years ago, my friend had marital issues and I wanted to help, but I was only able to provide a referral—something I had learnt in biblical school. I referred her to a counsellor, who invited me to sit with my friend, as her support during the session. Through a genogram (a pictorial display of a person’s familial relationships and medical history), carefully selected questions and active listening, she had a clear assessment of the issues my friend had brought up and provided options for my friend.
At the end of the session, the counsellor left the decision of her next steps to my friend. I was thoroughly impressed and that scene is etched in my mind. Sitting in during that session with my friend, an anxious woman looking for answers to her difficult marriage, inspired me to become a counsellor.
Was this your first job?
No. I used to work as a book keeper in a transport company. It is my love of helping people, that has kept me going as a counsellor, all these years.
Growing up, what did you want to be?
Growing up, I had simple dreams. I wanted to start a family and be a homemaker who raised good kids, because of my parents. I admired their perseverance, love and care for me and my eight siblings.
As a child, I was raised in a Taoist and Buddhist environment. I often felt stuck and frightened. Years later, I converted to Christianity and started being involved with my community. I devoted my time to ordinary clerical work before moving into pastoral work and eventually became a pastor in my church. In counselling school, I learned to help others and heal myself. Understanding my life story and personhood better was critical in my personal journey. Having understood myself better, I was then able to work with people in my community, like children with gender issues and couples with marital problems.
By helping my community, I also learnt a lot and became more aware of myself and my actions, my family and the world around me. But I wanted to do more. I wanted something different that would not only benefit my church community, but society at large.
I had initial doubts about my transition from pastoral work to my current work. It was a major decision and I did not want to make it on impulse. After months of meeting with my Leadership Transition coach for guidance, the career switch was successful, allowing me to become the Spiritual Care Counsellor I am today.
What are some of the reactions you usually get when you tell people what you do?
People often have the misconception that I am a morgue worker and are often surprised when I explain what I do. My siblings were initially quite fearful, as my job requires a lot of home visits, so they were worried that I would be in contact with diseases. This was more so during the COVID-19 pandemic. However, after explaining the nature of my work, they are now very supportive and appreciative of my contributions to the community.
How would you describe your job to someone who has never heard of it?
I often describe it in layman terms. In Chinese I would say, “治疗心病”, loosely translated to mean “treating diseases of the heart”. This would entail addressing topics such as religious beliefs, spiritual pains, the meaning of life or purpose of existence.
What are the expectations of being a Spiritual Care Counsellor?
It is important to be well-versed and understand the different religions and belief systems. As a Spiritual Care Counsellor, my job is to provide palliative pastoral care and counselling to patients, families, staff and volunteers where appropriate. Being sensitive and aware of the different religions and belief systems, allow me to better understand their perspectives and problems, to recommend the appropriate improvements.
It is also important to constantly improve and acquire skills of the modern age, to help our patients on their end-of-life journey. At this time, patients are often anxious and fearful of the unknown or death. Imparting techniques like mindfulness and breathing methods to patients, guides them to be at peace with themselves during this difficult time.
Finally, to provide education and information to patients with life-limiting illnesses, families and the public. My hope is to set up an open library that is equipped with relevant resources for everyone.
What is the best thing about being a Spiritual Care Counsellor?
It is the privilege of being able to enter a patient’s sacred space—their home—and journeying with them at the end of life. It is also a privilege to hear them share their dreams, wishes, pains, suffering, struggles and sometimes even secrets, that they do not even share with their loved ones in this sacred space.
What was one thing about the job that surprised you after you joined?
The dedication to our patients. Initially, I thought my job was to enter my patients’ homes and conduct my pastoral work quietly with them, but my colleagues have shown how they have gone above and beyond for our patients. They genuinely care very much for our patients and I am thankful to have this opportunity to witness and learn from them.
Describe what a day in your life is like.
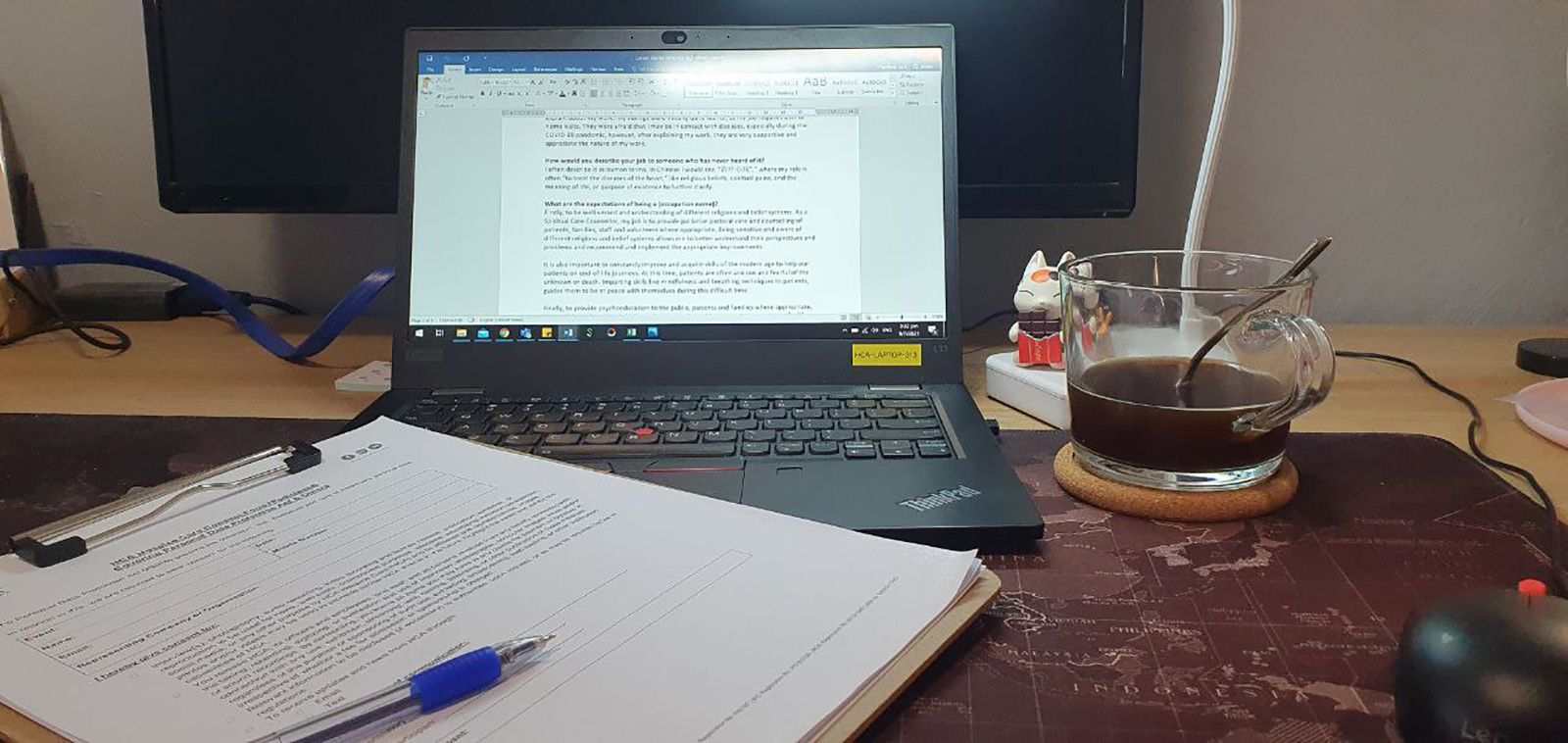
7am— During pre-COVID times, I would be on public transport heading towards the office. However, as we are now working from home, I prepare a cup of coffee to start the day and as I complete some administrative work.

8.30am – I check my emails, make a few phone calls to arrange for home visits or video consultation and prepare administrative work to conduct Family Dignity Interventions (FDI) with patients and families who are interested.
An FDI is a highly-focused meaning-oriented interview with patients and families, that is recorded, transcribed and edited into a legacy document for sharing with the patient and family.
9am – Some days, I cover our Vigil Angels when they are unavailable. Vigil Angels tend to patients’ basic bedside care, such as bathing or a change of clothes.


On other days, I would travel to my patients’ homes for a visit. Having to travel around the island while concurrently dealing with meetings, phone calls and other administrative work along the way can be tiring. I would usually cluster my home visits, so that I can reduce travel time. With the current safe management measures, I try to arrange for video conferencing, whenever possible.

10am—My first case of the day.

Patients and caregivers often share many things with me, from matters of the heart to their purpose in life, even religious and spiritual beliefs. I engage in active listening, while focusing on being empathetic towards them.
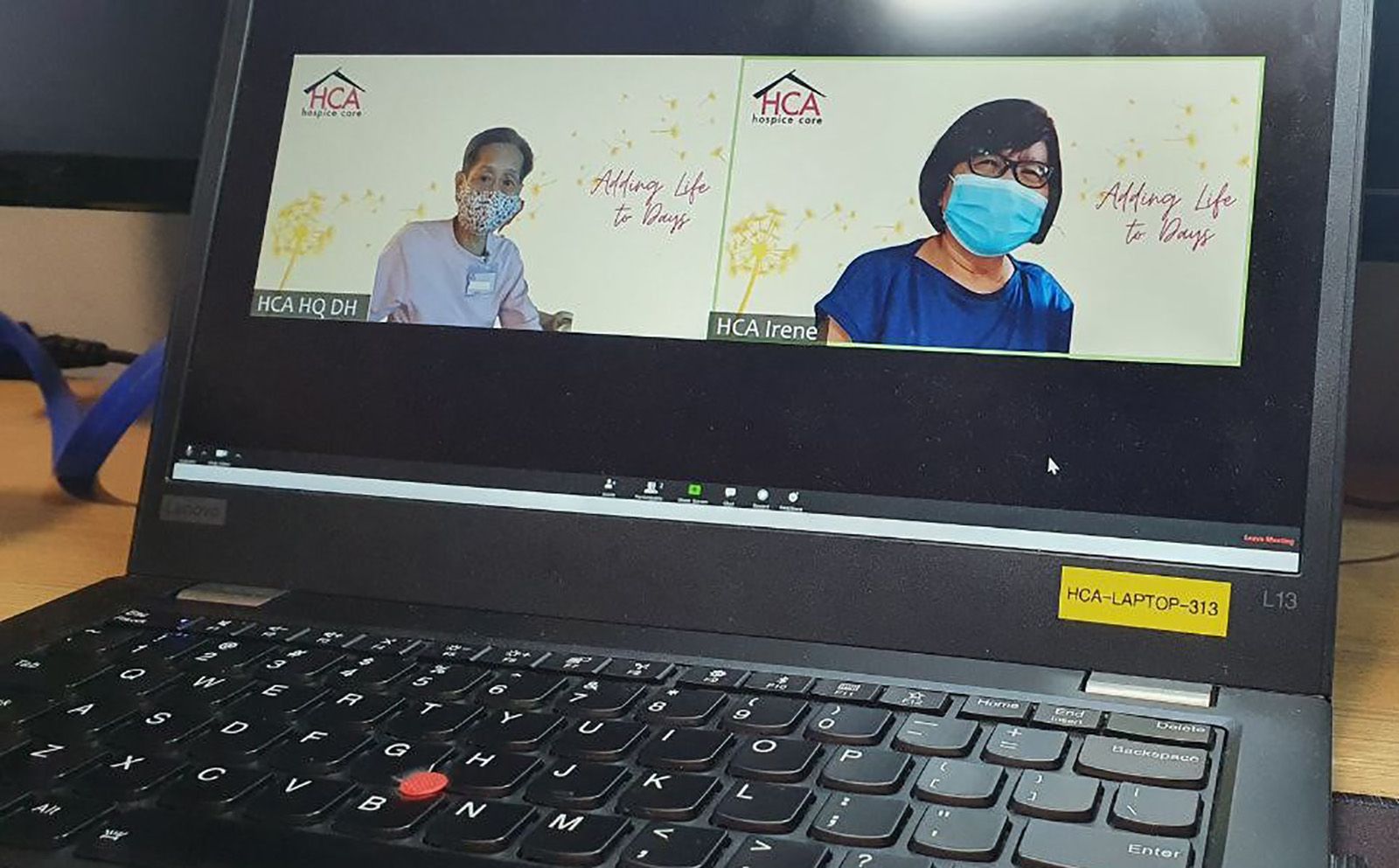
11.30am – After completing my first home visit, I check in on my Day Hospice patients via video call. We do this virtually now, to reduce any unnecessary exposure or cross contamination, per ministry guidelines.
12.30pm – Lunch. I take a break and recalibrate my mind and nourish my body. Once I am recharged, I am ready to continue my case work with our Day Hospice patients.

2.30pm – Psychosocial Services Case Supervision and tutorials. Some colleagues also share about the special cases they have encountered over the course of their work, to help us learn.

As a Spiritual Care Counsellor, I often interact with highly anxious patients and caregivers, who are quite emotional when sharing about their suffering. Some people look for comfort, while others look for advice; learning to differentiate these needs helps me put a smile on their faces. When I manage to help them in the way they need, it reminds me that I have chosen the right profession for myself.
5.30pm –Dinner time. Due to Covid-19, I have learned a few time-saving recipes that have reduced my cleaning time, freeing up time for me, to clear administrative work and pray and reflect on my day.

8pm –I go through the appointments for tomorrow and list down what I need to prepare. Knowing that I have everything down on my note book, I head for bed to watch my current favorite food shows or read. It might have been a long day, but I am all prepared to help more patients tomorrow.

